THEY are the everyday heroes now working around the clock to keep us safe from coronavirus.
And now NHS staff are facing one of the biggest tests of their careers, we want them to know how grateful the nation is for all they do.
Read our coronavirus live blog for the latest news & updates
With overworked staff having to take on extra shifts – and even being asked to come in when they are in self-isolation – and cut themselves off from loved ones to reduce any risk of infecting them, morale is at an all time low.
Here, five heroic staff members have revealed what life is really like on the frontline, with the threat of personal protective gear running out of stock, fears they and their colleagues could be infected at any minute, and over-stretched wards already nearing capacity.
‘We have one isolation bed – we won’t cope’
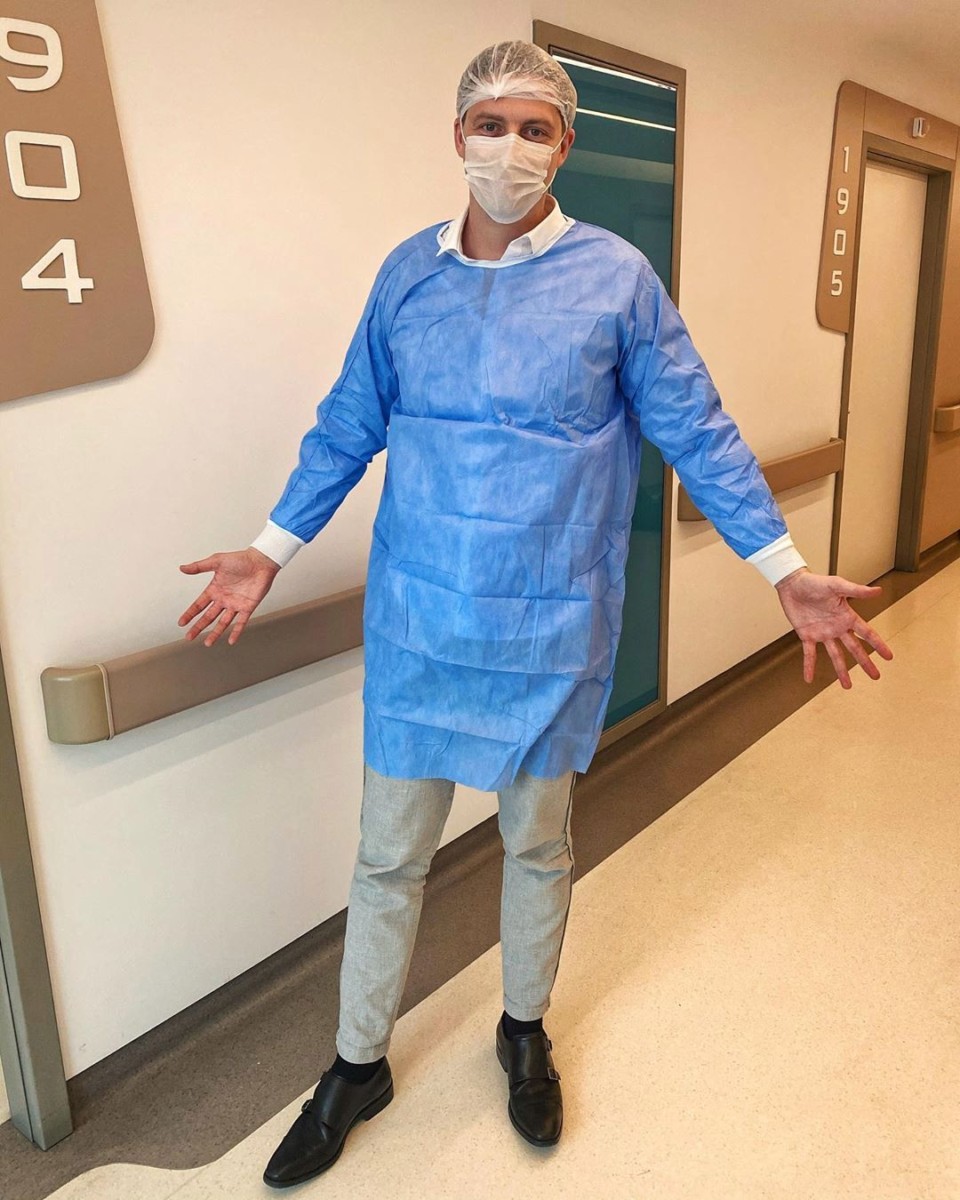
Former Love Island star Dr Alex George works in the Accident and Emergency department at University Hospital, Lewisham and says a big spike in cases could cause the NHS to buckle.

Dr Alex says: “I’ve been testing around eight patients a shift – and the NHS can easily cope with that level, but if we start seeing 50 or 60 a day, the pressure will be on.
The protective gear we have to wear at the moment adds to the queues at A&E.
Before seeing each patient I have to put on a gown, fit a mask and visor and double glove as well as the thorough hand-washing routine.
We have protocols for taking off the gowns… and we have to change our scrubs between each patient.
This is taking 20 minutes extra and tripling the time spent on each patient.
In our A&E department, we only have one isolation room for infectious diseases, with one bed, not the 15 or 20 beds you might imagine.
If numbers rise, we would have to quarantine whole wards.
It’s good the government is going to put more money in – but you can’t create more staff.
At the moment, frontline staff are being offered extra shifts and I know some who are working seven days a week.

In the short term, you can do that. If this was going to be around for a month, everyone could take on a couple of extra shifts.
But this looks like it will be around a good few months and it’s very difficult to sustain that over a period of time, as it becomes unsafe for people to work.
We have regulated hours because the longer you’re working, the more tired you become and the more likely to make mistakes.

What the NHS has always been good at is pulling together in a crisis. We are going to have to roll up our sleeves for the next couple of months until this settles, and morale is good at the moment.
But if this carries on for a long time, fatigue and stress will set in.
If over the next six months, one in five people have it we can deal with it. But if four in five people catch it, the NHS simply can’t cope.”
‘Staff are being asked to self-isolate – then called in because we’re too desperate’
Dr Rinesh Parmar, 31, is a speciality registrar in anaesthetics and intensive care in the West Midlands.

Dr Parmar says: “It’s feeling really under pressure at the moment and there are frantic plans being made to try and prepare us.
We’re testing patients every day, but it takes over 48 hours for us to get a result.
We have to assume anyone with breathing symptoms is positive and treat them as such – that’s increasing the workload dramatically.
My colleagues are really stretched. There’s obviously so much pressure, but the problem we have is there’s a background of pretty low morale within the NHS anyway.
Tap to see where COVID-19 is near you

We’re already short of staff on any given normal day without the pressure of the pandemic.
The NHS has a tremendous ability to instil camaraderie amongst staff, but that’s really being tested at the moment because we all have our own anxieties.
My parents are elderly, and they would be in the category where they’ve got underlying health problems, so I’ve stopped seeing them completely.
Naturally we’re more susceptible to this, and because we don’t know who’s positive and who’s not, you could come across a patient, be treating them, and not be wearing the full protection.

The other worry for doctors is that we’re being told there may be a rationing of personal protective equipment.
Plus, the advice for the public [if they come into contact with someone who’s infected] would be to self-isolate for seven days.
But what’s happening with NHS staff is they start self-isolating, but then many of them have had a phone call asking them to come back into work… potentially becoming a risk to patients and other staff.
They’ve spoken about cancelling annual leave for staff. That hasn’t happened yet but they’re compiling a list of volunteers.
There’s also plans in place to redeploy other doctors, such as GPs, and bringing retired doctors back too.
I worry that we’re leaving this too late for us [UK] to go into lockdown.
We’re pretty full and although we can find physical space, the problem is we don’t have the staff.
The government have said they’ll try to get more ventilators made, which is great and shows they’re listening, but we need healthy staff to come into work to be able to operate them.
Our view is that if you prioritise the testing of staff, then those of us that are negative can come back and we don’t have to self-isolate for seven days.
Day by day we’re getting more and more prepared, but the problem will come when we’re overwhelmed on the unit and we’ve got staff going off sick. Then we’re really struggling.”
‘There are no obvious solutions’
Dr Yaso Browne is a GP in a practice in Southampton.

Dr Browne says: “As we hear of more cases, our colleagues being affected, and knowing that we don’t have sufficient personal protective equipment, it makes us feel vulnerable.
We support the efforts that are out there, but we’re all a bit fearful – we’re not currently being allowed to be tested unless we’re symptomatic.
Also, if we are, then actually we don’t get the test back in very good time.
I think a bit more understanding about the testing, its supply, and what the capacity is would be hugely beneficial.
For now, I think the feeling is we’re feeling vulnerable, rather than stressed. I sense people wanting to do something positive to try and help make us feel stronger, for our patients and for ourselves.

I’ve actually chosen to limit my interactions with other people, because I’m worried that I’m high risk – so particularly limit interactions with those that I identify as more at risk.
I think really it’s just more about trying to reduce the potential that you’re transmitting to family members. I do have loved ones that I’d worry about because they are at risk.
But that’s also why you’d want to know if you’ve had COVID, because then you’d probably be more able to have those social interactions.
We haven’t seen any obvious solutions yet, so it is a really worrying issue for all of us.”
‘It’s hitting home that it’s really very serious now’
Leaanne Pallant is a 35-year-old agency nurse in Hertfordshire. She is married to teacher Richard, and has two children, Poppy, seven and Isla, nine.

She says: “On Sunday I worked on an isolation ward where 15 patients were being tested for the virus and a few were struggling to breathe.
There was one case of coronavirus in the hospital at that time, in the Intensive Care Unit (ICU), and one case on our ward who was strongly suspected of having it.
It was quite scary seeing the specialists dressed in the full-on protective gear. It really hit home that this is getting pretty serious now.
All the patients are in separate isolation rooms and nurses or healthcare professionals are having to glove and gown and mask up before we go into that room.
Then we have very strict degloving, taking your apron off and then washing your hands in a particular way, to protect yourself.

We also have to have a runner so we don’t have to take everything off if we need something brought in, and drug charts are banned, so we’re almost doing patient identification through the window before administering drugs.
The NHS was stretched before this, but the coronavirus is putting extra strain on it.
As an agency nurse, who fills in on an ad hoc basis, there are a ridiculous amount of shifts being advertised out and a lot of people don’t want to put themselves in that situation.
So nurses are actually cancelling extra shifts that they don’t have to be doing.
I don’t worry about myself catching the virus because I’m 35 and I think my immune system is pretty tip top, and the children don’t have any underlying health issues.
But I have an elderly nan who I try and see once or twice a week. I’ve had to say to her, ‘Sorry Nan if you need me to do an online shop for you I will but other than that, I’m not going to be coming to see you,’ because I could have it and not know.
I would never forgive myself if I gave it to her. So there is a lot of trying to distance myself and just be sensible, under the circumstances.
As nurses, we’re exposed to a lot of bugs and viruses and it’s part and parcel of the job but this is an unknown virus so there are a lot of questions we don’t know the answer to.
I went to do my normal weekly shop today and there’s literally nothing on some shelves. It was post-apocalyptic.
But life has to go on, and all we can really do is try and protect the people that need protecting.
The country as a whole is doing what they can and what they need to do.
I just hope that everybody is understanding and does isolate if they need to rather than being stupid about it. Because it could be those few stupid people that ruin it for the majority.”
‘If this was a one-off event, we’d all be called in’
Dr Robert Hirst, 31, works as an emergency medicine trainee in Bristol.

He says: “We have a few COVID patients here now, and there’s a few more coming in.
We’re cancelling elective surgeries from Thursday here and just moving to emergency and cancer surgeries primarily.
We’ve been told we’re going to be redeployed to whoever needs us in the coming weeks – I imagine I’ll be moving into the emergency department or intensive care soon.
It’s tense at the moment, it’s quite unknown and we all sort of feel like we’re at the beginning of something… it’s probably going to get worse before it gets better.
I’ve seen emails from other trusts saying the previous advice given doesn’t apply to healthcare workers… but luckily no-one has been called in here from self-isolation yet.
It’s going to be a prolonged process here, it could be six months, there could be another peak in the winter, they’re having to be more sustainable with this.
If this was a one-off major event, we’d all be called in and it would be all hands on deck for a few days, but this is longer.
A main concern for me is I live with my girlfriend and I’m worried I could bring my work home with me in a very unpleasant way.
Fundamentally we’d be fine, but it’s the chance we could pass it on to my grandparents. We were supposed to meet them this weekend for my birthday but we’re having to hold off.
Normally when you suit up it’s protection for the patients, but now it’s protection for the patients and for yourself and anyone else you come into contact with.
I know a lot of people are concerned and we hear lots of rumours of young doctors being ill or in intensive care, or even have passed away, so I know it’s something that weighs on people’s lives.
This very much could go downhill, but we just don’t know yet.”
‘There is fear among clinicians too’
Dr Murray Ellender is a London GP and co-founder of eConsult.

“GPs are having to think about fundamentally changing the way we work, and coming up with ways of managing the patients without them necessarily coming into the building.
It’s disrupting the model of general practice – which is probably not a bad thing – but it’s happening faster than we would have expected or hoped.
There’s a lot of worry about coronavirus and people with respiratory symptoms, but we’ve also got the everyday general practice with people coming in needing repeat prescriptions or with other health conditions.
We’re having to manage the normal day job as well as people presenting with respiratory problems.
It’s putting all sorts of pressures on the system and there’s the added concern of how we look after the workforce.
If you’ve got a practice that’s got four or five GPs, you might have one who’s pregnant who’s now been advised they shouldn’t be at work, what impact does that have on the rest of the practice staff?
We’re having to manage increased demand with perhaps a slightly diminished workforce.
Most GP practices, which have around 7,000 patients typically, are now looking at how they can work together when doctors are having to go into isolation.
I’ve got a couple of colleagues who’ve had confirmed coronavirus. One of my partners is Clare Gerada, who’s been in various press at the weekend talking about her experience of the illness.
We have others who are now in isolation because they’ve either got symptoms or are pregnant.
What we’re thinking through now is, ‘How can we still make use of their expertise and get them working from home?’
Anyone who is in isolation who is feeling well enough to work can use a laptop to deal with certain patient queries remotely. And actually that helps them support the wider system.
The system we founded, eConsult, is used in around 1,400 practices across the UK with half of all practices using that or a similar online consultation system.
But half the country has nothing and the NHS is scrambling to make online consultation available to everyone.
Practices are now asking, ‘How can we get this? And fast?’
Last year, we were bringing about 50 practices a month on board. In the last couple of weeks, we’ve been bringing about 50 practices a day. It’s just gone nuts.
There is a certain amount of fear amongst clinicians as well as the general public.
We have some who’ve got long-term conditions or are the carers for elderly relatives.
As so often happens, we don’t do enough in any society to look after healthcare workers. And they don’t tend to be very good at being looked after either – they tend to make very bad patients!”